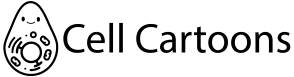
The tumor microenvironment (TME) is the complex “neighborhood” of cells and structures that surround and interact with a tumor. It includes not only cancer cells but also many non-cancerous cells and support structures that influence how the tumor grows and behaves. This environment and the tumor constantly communicate with each other, shaping disease progression.

Below are more detailed explanations about the cells and interactions that are shown in the full illustration.
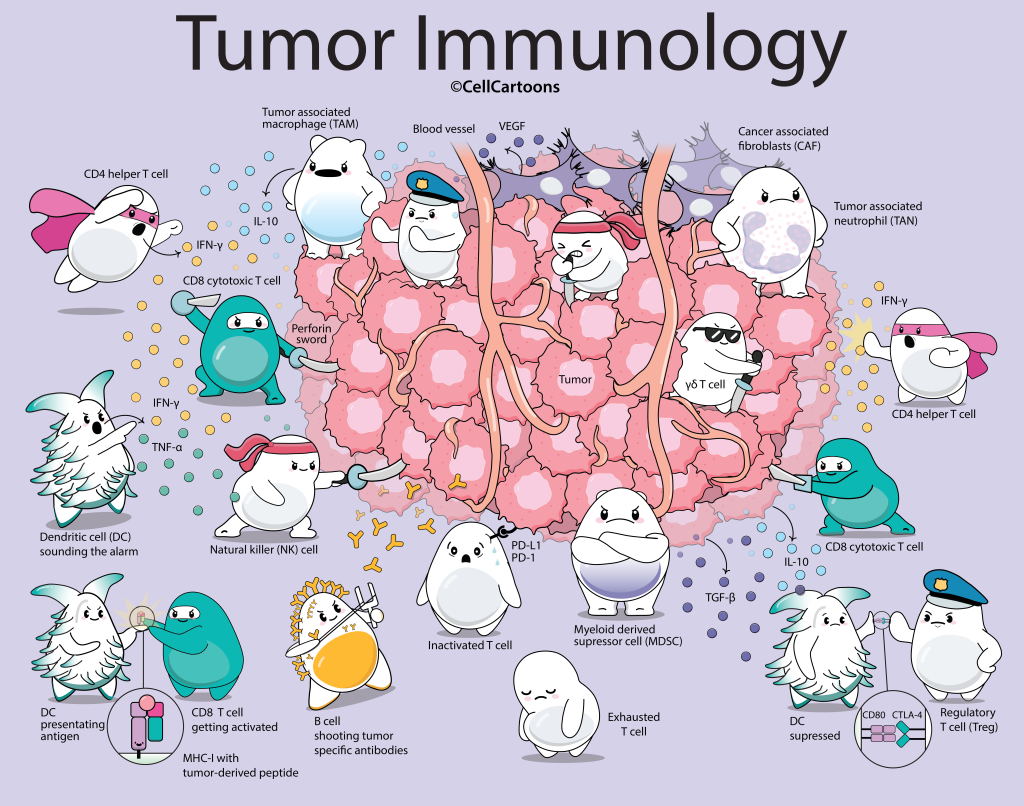
CD4 Helper T cells are immune cells that act as coordinators of the immune system within the tumor environment. These cells release cytokines like IFN-γ and play a critical role in helping to activate both CD8+ T cells and B cells.
CD8 Cytotoxic T cells are another subset of T cells but they have the power to kill. They are the immune system’s primary executioners. They use several proteins to kill cancer cells including perforin, a pore-forming protein. Through the pore the cells transfer other proteins like granzymes, which initiate a cascade of events that lead to the target cell’s death through apoptosis.
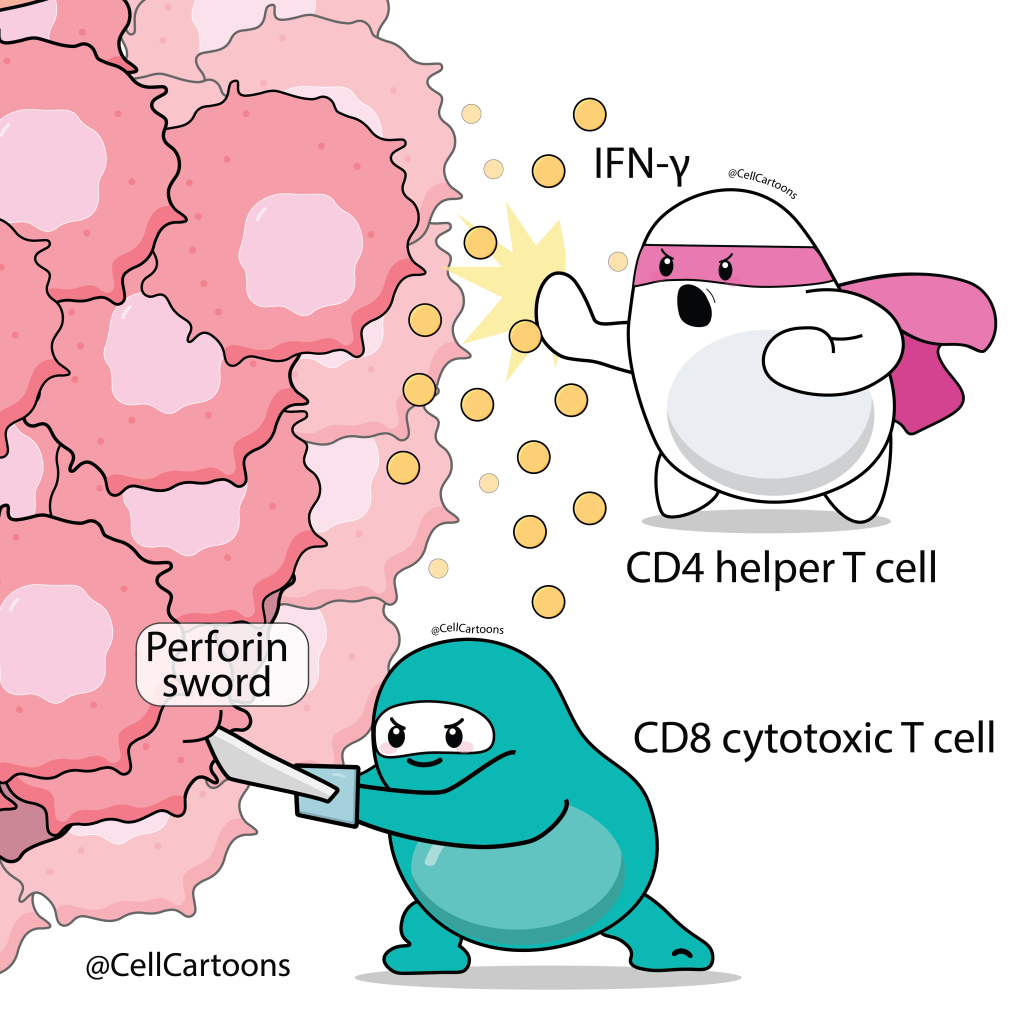
Dendritic cells (DCs) are specialized immune cells that activate the T cells. They are known as professional antigen-presenting cells (APCs) and they act as “scouts,” capturing pieces of the tumor called antigens. They then present these antigens to CD8 and CD4 T cells using major histocompatibility complexes (MHC) Class I and Class II, respectively.
The DCs present the MHC I and II with the peptide (shown in pink) on their cell surface. The T cells with a compatible T cell receptor (TCR) get activated.

Antigen presenting cells like DCs and macrophages secrete pro-inflammatory cytokines like IFN-γ and TNF-α. These cytokines help other cells get activated to fight the tumor.
B cells produce specific antibodies directed against the tumor. These antigens are also called tumor specific antigens. The antibodies that recognize the tumor antigens can help fight cancer by marking tumor cells for destruction, enabling immune cells to carry out antibody-dependent cellular cytotoxicity (ADCC).
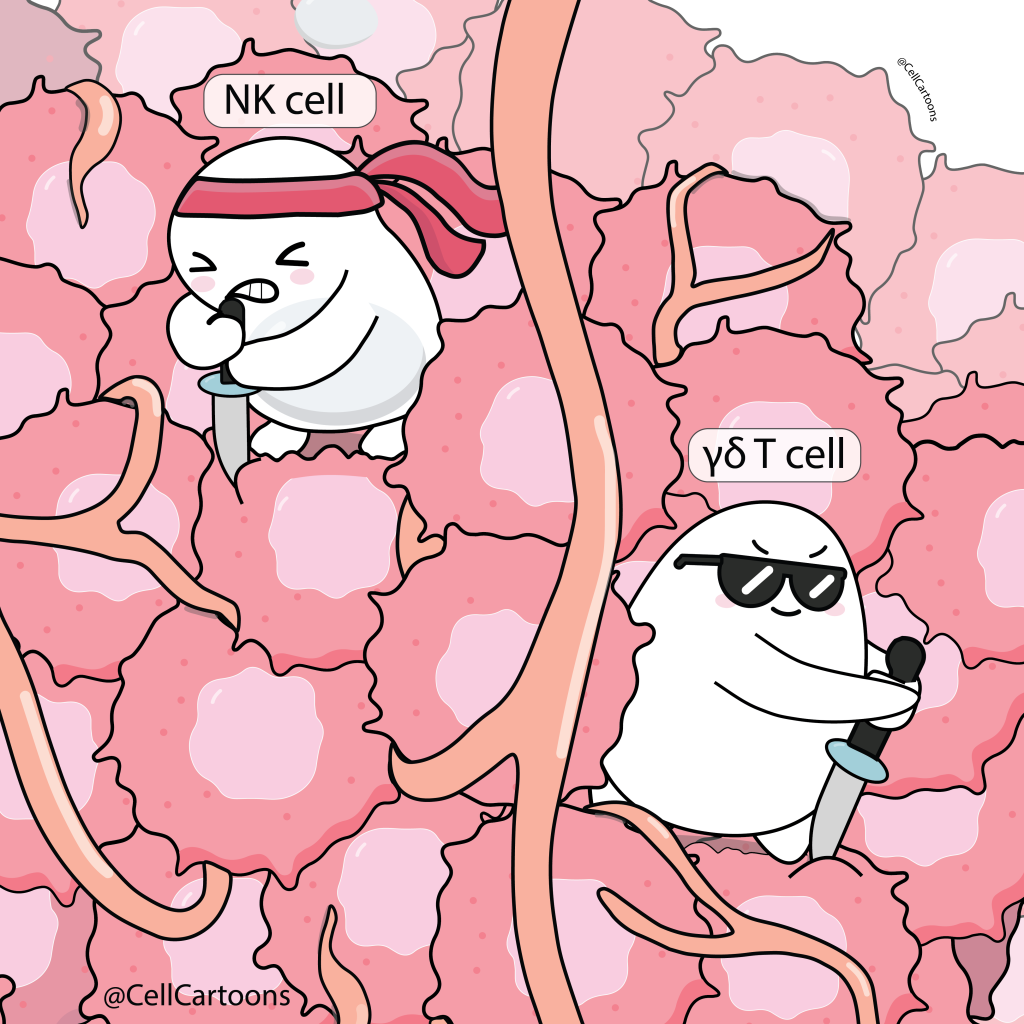
Natural killer (NK) cells and Gamma delta (γδ) T cells are other important immune cells that have the ability to kill. These cells infiltrate the tumor and kill cancer cells.
NK and γδ T cells are being investigated and actively developed as candidates for cell therapy treatments against cancer.
Macrophages, neutrophils and myeloid cells are other types of immune cells that normally help us fight the ‘bad guys’.
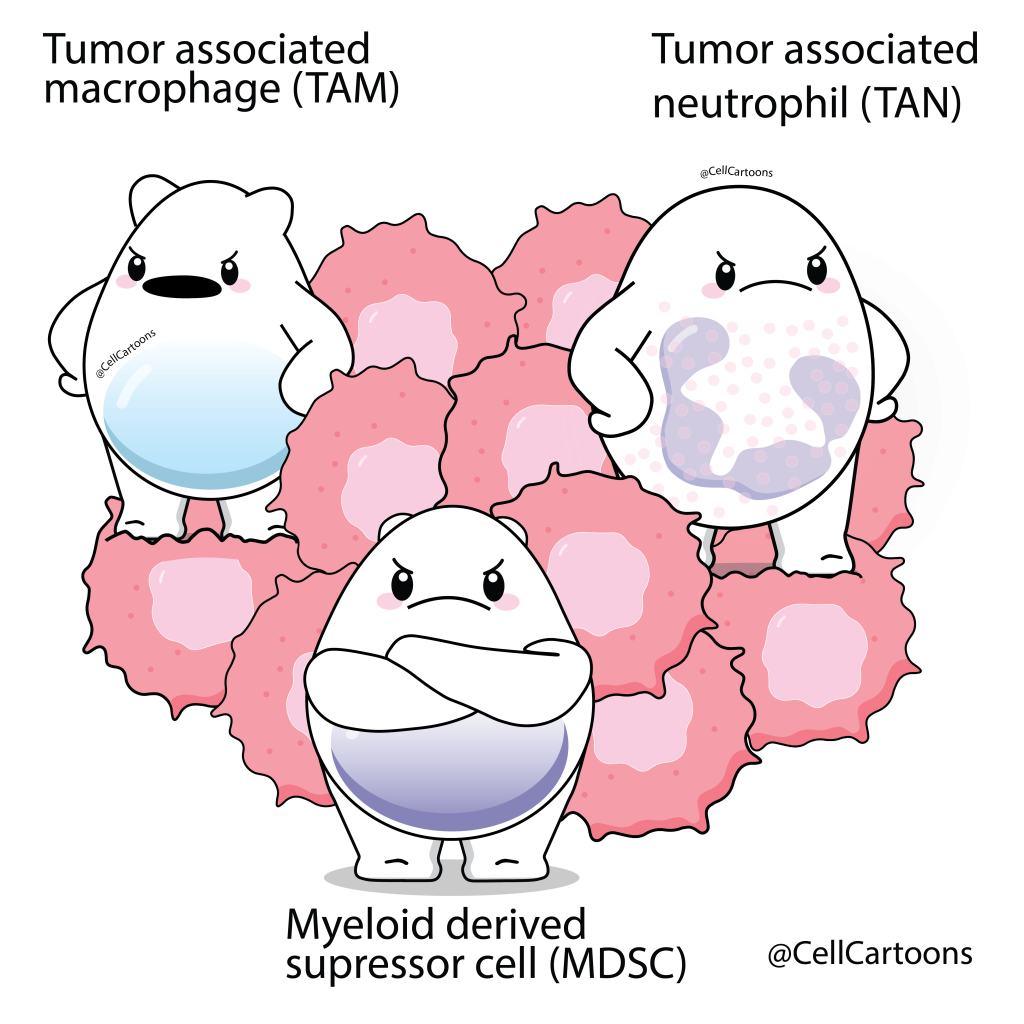
However, in the tumor environment the tumor-associated macrophages (TAMs) usually known as M2 macrophages, tumor-associated neutrophils (TANs), and myeloid-derived suppressor cells (MDSCs) have been reprogrammed by tumors to suppress immune responses and help protect the cancer cells.
TAMs secrete inhibitory factors like IL-10 and both, TAMs and TAN release growth factors that promote the growth of new blood vessels (angiogenesis), helping tumors grow and spread.
Regulatory T cells, or Tregs, help to dampen the immune response, and in cancer this can work against us.
Tregs may express high levels of immune checkpoint molecules such as CTLA-4 and PD-1, which they use to silence nearby DCs. When CTLA-4 binds to CD80 on the DC, the DC can no longer use CD80 to activate other T cells against cancer. CTLA-4 can also trigger trans-endocytosis, pulling CD80 off the DC surface and leaving the dendritic cell unable to send activation signals at all.

To evade the immune response some tumor cells can express a Programmed Death-Ligand 1 (PD-L1).
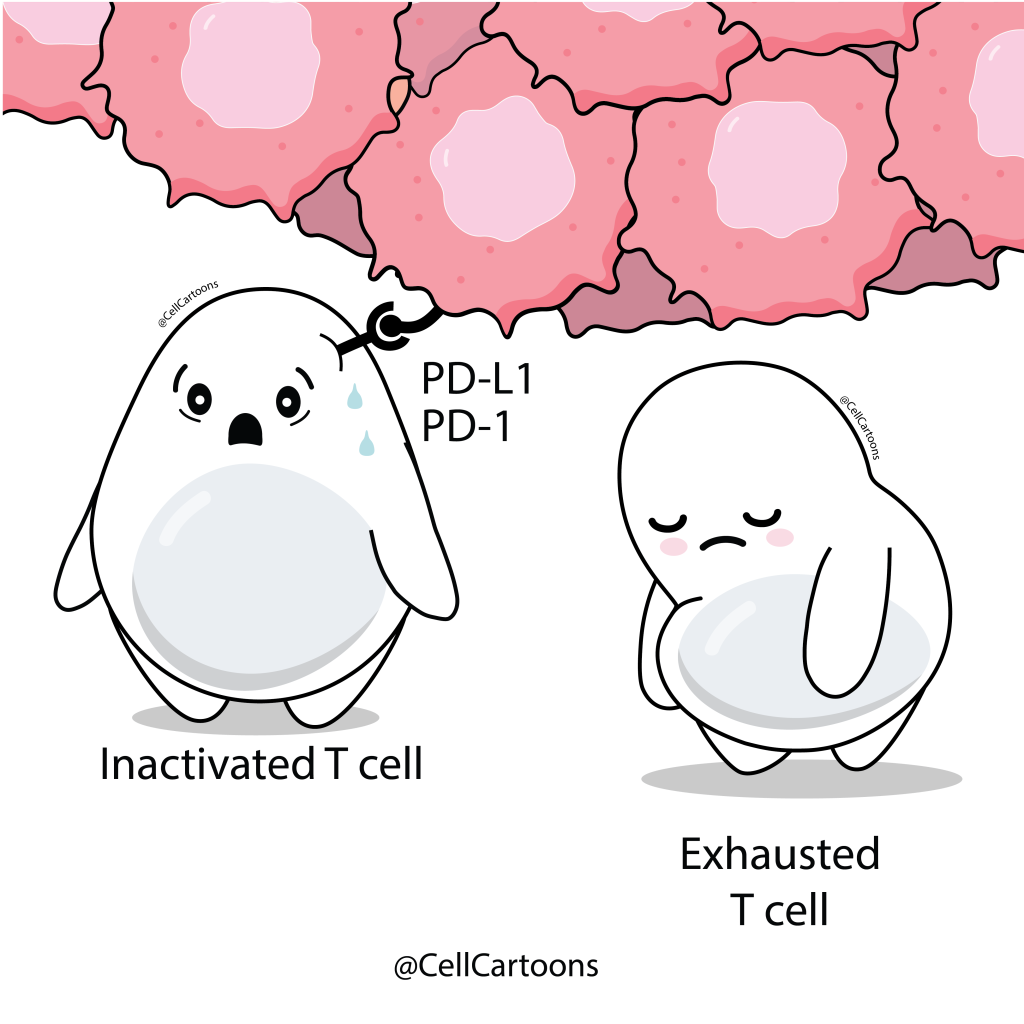
PD-L1 binds to PD1 on T cells and supressess them and causing T cell exhaustion. When T cells are exhausted they lose their cytotoxic effectiveness and ability to replicate.
PD-L1 is expressed by tumor cells as an immune-evasion mechanism and can also be expressed by other cells in the TME including, TAMs, TANs, and Tregs.
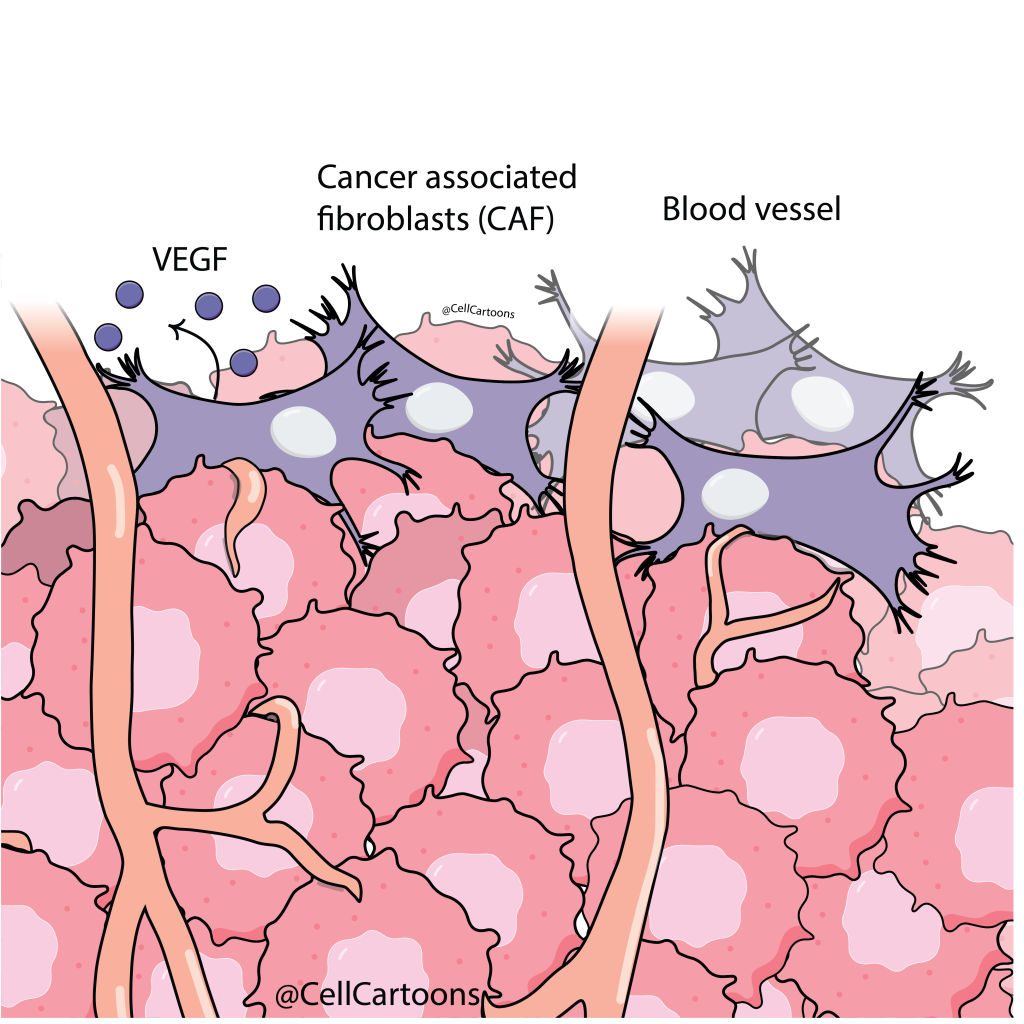
Cancer-associated fibroblasts (CAFs) are key stromal cells in the tumor environment that promote tumor growth and therapy resistance.
CAFs secrete a special protein called vascular endothelial growth factor (VEGF). This protein stimulates new blood vessel formation, weakens dendritic cell function, and supports tumor survival, invasion, and spread.
CAFs block T cells by secreting factors like TGF-β and remodel the extracellular matrix to create dense tissue that limits drug delivery.
The TME is highly complex, and every tumor is unique, yet many share common immune-evasion mechanisms that researchers are steadily uncovering. These insights have led to new therapies, including antibodies that target PD-1 and CTLA-4, such as Keytruda and Yervoy. There are new emerging approaches like:
These are now pushing the next wave of innovation in cancer treatment.

References
- Barker H, Paget J, Khan A, et al. The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nature Reviews Cancer. 2015;15:409–425. https://doi.org/10.1038/nrc3958
- Ghebremedhin A, Athavale D, Zhang Y, Yao X, Balch C, Song S. Tumor-associated macrophages as major immunosuppressive cells in the tumor microenvironment. Cancers. 2024;16(19):3410. https://doi.org/10.3390/cancers16193410
- Glabman RA, Choyke PL, Sato N. Cancer-associated fibroblasts: tumorigenicity and targeting for cancer therapy. Cancers. 2022;14(16):3906. https://doi.org/10.3390/cancers14163906
- Gomes S, Rodrigues AC, Pazienza V, Preto A. Modulation of the tumor microenvironment by microbiota-derived short-chain fatty acids: impact in colorectal cancer therapy. International Journal of Molecular Sciences. 2023;24(6):5069. https://doi.org/10.3390/ijms24065069
- Mensurado S, Blanco-Domínguez R, Silva-Santos B. The emerging roles of γδ T cells in cancer immunotherapy. Nature Reviews Clinical Oncology. 2023;20:178–191. https://doi.org/10.1038/s41571-022-00722-1
- Shaul ME, Fridlender ZG. Tumour-associated neutrophils in patients with cancer. Nature Reviews Clinical Oncology. 2019;16(10):601–620. https://doi.org/10.1038/s41571-019-0222-4Silvestre-Roig C, Kalafati L, Chavakis T. Neutrophils are shaped by the tumor microenvironment: novel possibilities for targeting neutrophils in cancer. Signal Transduction and Targeted Therapy. 2024;9:77. https://doi.org/10.1038/s41392-024-01786-4
- Tay RE, Richardson EK, Toh HC. Revisiting the role of CD4+ T cells in cancer immunotherapy: new insights into old paradigms. Cancer Gene Therapy. 2021;28:5–17. https://doi.org/10.1038/s41417-020-0183-x